On July 12, the Centers for Medicare & Medicaid Services (CMS) published its 2019 Medicare Physician Fee Schedule Proposed Rule (Proposed Rule) covering a wide range of topics. In our series of articles, we have summarized and offered our insights on several key provisions. Note that comments on the Proposed Rule were due to CMS by September 10, 2018, and we expect CMS to publish the Final Rule later this fall. Of the 15,313 comments CMS received on the Proposed Rule, 1,212 of them included the acronym MIPS. You can review all the comments here.
In addition to the usual updates to Part B payment policies, the Proposed Rule includes numerous changes to the Quality Payment Program (QPP). With regard to MIPS—the Merit-Based Incentive Payment System—CMS continues to implement the program per statutory requirements, while streamlining processes and reducing burden.
The following summarizes the seven most important proposed changes to MIPS’s scope and application. In a separate article, we will address CMS’ proposed changes to the specific performance measures in each of the four MIPS categories (Quality, Cost, Improvement Activities, and Promoting Interoperability—formerly known as Advancing Care Information—which was the successor to Meaningful Use).
For those wishing to take a deeper dive, CMS has published a 28-page fact sheet detailing its proposed changes to the QPP for 2019.
1. Performance Categories and Thresholds. For the 2019 performance year, CMS proposes to re-weight the performance categories as follows:
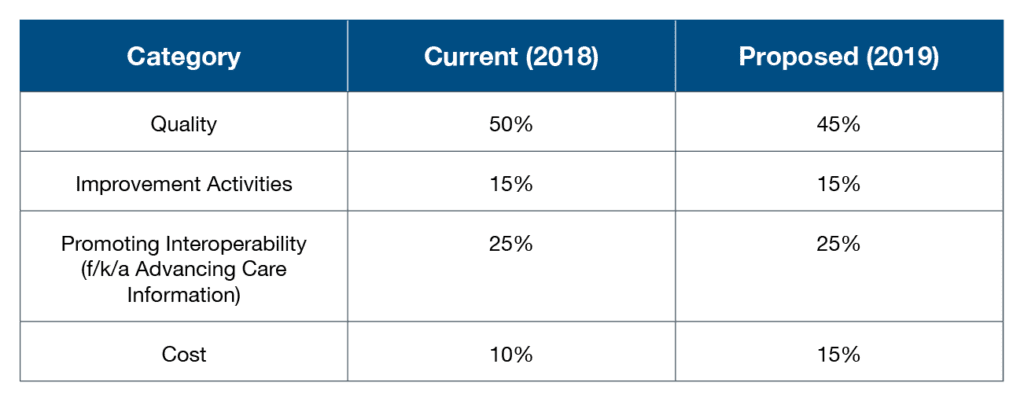
CMS proposes to increase the performance threshold (the score a provider must achieve to avoid a downward adjustment) from 15 points to 30 points. As a result, more providers are likely to face penalties in 2021 based on 2019 performance. CMS also intends to set the exceptional performance threshold (the score a provider must achieve to participate in the exceptional performance bonus pool) at 80 points. The proposed reporting periods for each performance category remain the same at 12 months for quality and 90 days for Improvement Activities and Promoting Interoperability.
For 2017 and 2018, providers could submit information for only one performance category and still avoid any penalty. In 2019, however, the increase in the performance threshold means participation across multiple performance categories, or optimal performance in the Quality performance category, will be necessary to avoid any penalty.
2. Part B Drugs. MACRA, the Medicare Access and CHIP Reauthorization Act, required MIPS payment adjustments be made to payments for both items and services under Medicare Part B, including Part B drugs. However, the Bipartisan Budget Act of 2018 limited MIPS payment adjustments to professional services only. CMS proposes to implement this legislative mandate effective January 1, 2019. This means there will be no payment adjustments for Part B drugs or other items based on 2017 performance.
3. Eligible Clinicians. CMS proposes that physical therapists, occupational therapists, clinical social workers, and clinical psychologists become Eligible Clinicians in the 2019 performance year. CMS is also considering adding qualified speech-language pathologists, qualified audiologists, certified nurse-midwives, and registered dieticians in 2019. However, CMS’ proposed revisions to the performance metrics in the Quality category will likely result in a limited number of measures that apply to the latter group. If that number falls below six (which is expected), CMS intends to delay to a future performance period this group’s inclusion.
CMS proposes to assign 0% weighting to the Promoting Interoperability category for these new Eligible Clinicians, resulting in a re-weighting of the other categories. For purposes of group reporting, the inclusion of these additional providers may significantly impact total performance scores if a practice has not implemented processes across its entire organization.
4. Low-Volume Threshold and Opt-In. Presently, an Eligible Clinician or group is excluded from MIPS participation if the clinician or group (1) has less than $90,000 in Part B allowed charges, or (2) treats fewer than 200 beneficiaries. For 2019, CMS proposes to also exclude an Eligible Clinician or group that provides fewer than 200 covered professional services.
CMS also proposes that an Eligible Clinician or group that would be excluded under the low-volume threshold may “opt in” to MIPS participation, voluntarily subjecting themselves to the reporting requirements and payment adjustments. However, those Eligible Clinicians and groups that meet all three exclusion criteria (amount of allowable charges, number of beneficiaries, and number of services), could not “opt in” to the payment adjustments; they would be limited to voluntary reporting and receive a MIPS score for comparison purposes only.
5. Facility-Based Scoring. CMS proposes a new facility-based scoring option that would not require additional data submission. Facility-Based Clinicians are Eligible Clinicians with 75% or more of covered professional services provided in an inpatient setting. A group qualifies as a Facility-Based Group if 75% or more of its Eligible Clinicians are classified as Facility-Based Clinicians.
Under CMS’ proposal, a Facility-Based Clinician would be attributed to the hospital at which he or she provides the most Medicare services. Facility-Based Groups would be attributed to the hospital to which a plurality of its Facility-Based Clinicians is attributed.
The Value-Based Purchasing score of the attributed hospital would be used to determine its Facility-Based Clinicians’ and/or Facility-Based Groups’ scores in the Quality and Cost performance categories. No additional reporting would be required for Facility-Based Clinicians. Facility-Based Groups, however, still would be required to report under the Improvement Activities or Promoting Interoperability categories.
6. MIPS Determination Periods. CMS is proposing to use the same MIPS determination period for the low-volume threshold, non-patient facing, small practice, hospital-based, and ASC-based criteria: an initial 12-month period beginning October 1 through September 30 of the calendar year preceding the performance year and a second 12-month period beginning October 1 and ending September 30 of the performance year. The second 12-month period would include quarterly snapshots to assist the provider in determining eligibility status sooner.
Streamlining the determination periods will allow CMS more time to evaluate data and potentially communicate MIPS reporting status earlier. It will also create less confusion in the evaluation timeframes for each area.
7. Virtual Groups. CMS proposes a new virtual group determination period: the 12 months ending September 30 of the year prior to performance year. This timing will align with the first portion of the MIPS determination period, allow more time for CMS to determine TIN size, and communicate in a timelier manner regarding status with potential Virtual Group participants prior to election. Those considering the Virtual Group option will be able to inquire about status through the QPP service center.
PYA assists providers in navigating the complex MIPS requirements and maximizing performance. Contact a PYA executive below for more information at (800) 270-9629.
© 2018 PYA
No portion of this article may be used or duplicated by any person or entity for any purpose without the express written permission of PYA.


