Executive Contacts
On March 8, 2022, the Centers for Medicare & Medicaid Services (CMS) provided additional guidance on Section 131 of the Consolidated Appropriations Act regarding teaching hospitals’ eligibility for direct graduate medical education (GME) resets. The article below has been updated with this additional information.
For more than two decades the United States has been under a congressionally imposed cap on federal support for GME. The Balanced Budget Act froze Medicare support for increased GME slots at 1996 levels. Recently, CMS announced its first funding for new residency slots since the act became law in 1997.[i] Medicare is the largest public contributor of GME funding, making this announcement even more impactful.
Through legislation enacted as part of the Consolidated Appropriations Act of 2021 (the Act), the new funding will provide an estimated $1.8 billion from FY 2023 – FY 2031 for 1,000 new GME residency training slots. The application and criteria can be found here.[ii] The initial application deadline is March 31, 2022, for the first round of funding. For this round, CMS will notify a hospital about an approved increase by January 31, 2023, for funding available for FY2023 starting July 1, 2023. Hospitals seeking relief through additional cap slots will be required to complete their applications and submit them through the MEARIS system.
Section 126 of the Act outlines the following distribution for the new slots, including the following categories:
- Rural Hospitals – this category covers hospitals located in a rural area or classified as located in a rural area for acute inpatient payment purposes.
- Resident Cap Relief – this category covers hospitals with very low resident full-time equivalent (FTE) caps and per resident amounts–sometimes inadvertently or unknowingly set. The application deadline for this category is July 1, 2022.
- States With New Medical Schools – this category covers states with a new medical school as of January 1, 2000. This includes 35 states and 1 territory: Alabama, Arizona, Arkansas, California, Colorado, Connecticut, Delaware, Florida, Georgia, Idaho, Illinois, Indiana, Kansas, Kentucky, Louisiana, Massachusetts, Michigan, Mississippi, Missouri, Nevada, New Jersey, New Mexico, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, Puerto Rico, South Carolina, Tennessee, Texas, Utah, Virginia, Washington, West Virginia, and Wisconsin.
- Hospitals Serving or in a Health Professional Shortage Area (HPSA) – this category covers hospitals in designated HPSAs.
This new funding also comes at a time when the shortage of physicians is expected to exceed 139,000 by 2033, according to The Complexities of Physician Supply and Demand: Projections from 2018-2033—the sixth annual study issued by the Association of American Medical Colleges (AAMC).[iii] The impact of the COVID-19 pandemic is expected to accelerate this number beyond the top of the projected range.
These additional slots provide a great first step to adding much-needed training. According to the National Resident Matching Program (NRMP), 42,508 DO and MD graduates applied for 38,106 resident positions in the 2021 Main Residency Match. The NRMP now covers more than 96% of all physicians entering GME in the United States since the DO and MD residency programs became fully merged at the end of 2020.[iv]
Data has long shown the correlation between medical student education, residency training, and the eventual practice site chosen by a physician. The most recent report published by the AAMC shows that “overall, 57.1% of the individuals who completed residency training from 2011 through 2020 are practicing in the state of residency training.” The complete report can be found here.[v]
Hospitals hoping to address physician shortage issues in their service area would be well-served to consider using this new legislation to help advance their physician supply strategy. Existing teaching hospitals should first determine under which of the four categories their hospital may qualify. Teaching hospitals should confirm eligibility as an HPSA, identify and prioritize programs that may qualify for funding, and submit the applications before the round-one deadline of March 31, 2022. If a hospital is not an existing teaching hospital, it should consider the feasibility of becoming one as part of this initial but immediate strategy.
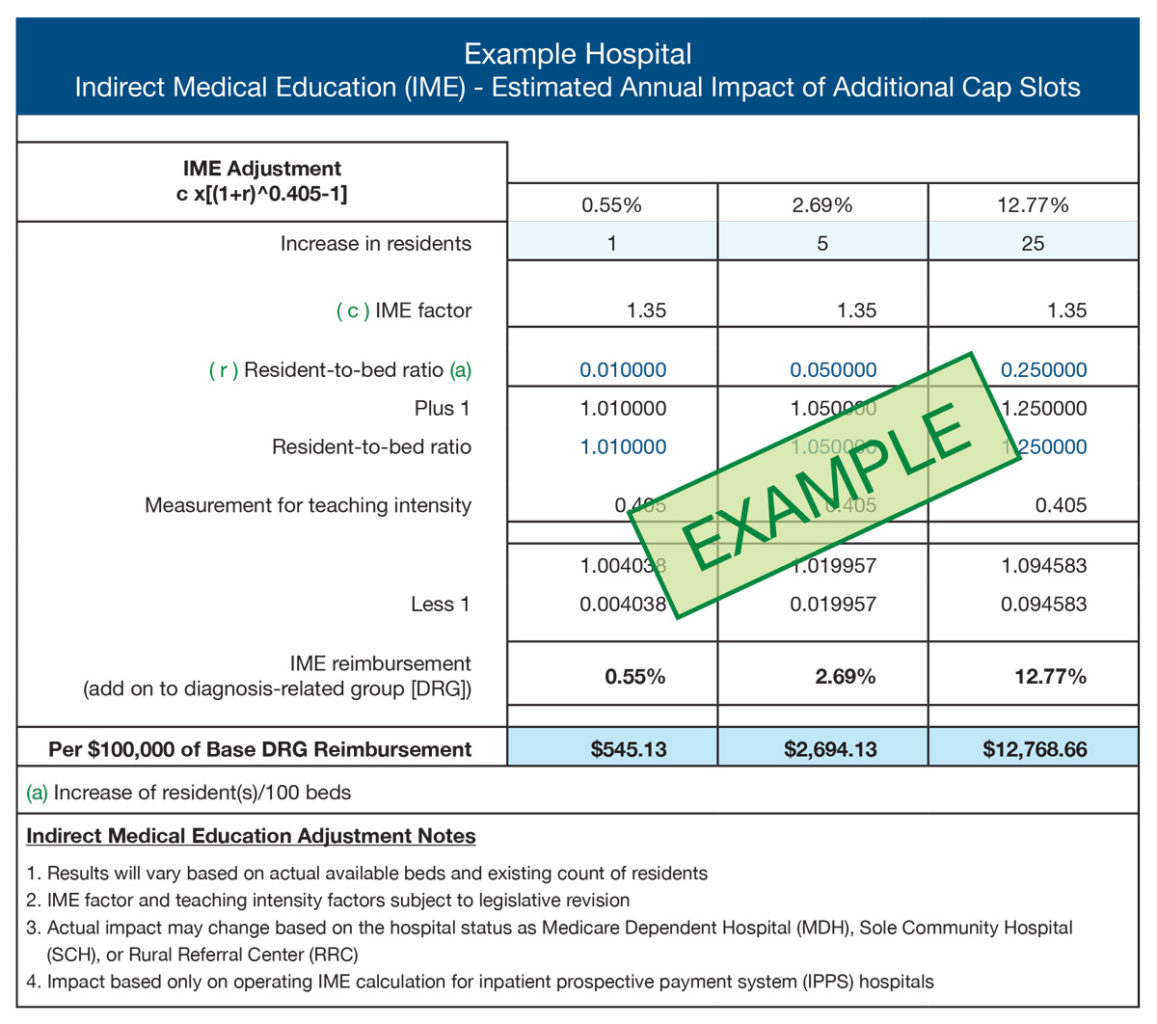
The new CMS program is set to have five rounds of funding. It is possible for a hospital to focus on a later round of funding as a strategy to help meet its physician shortage needs by creating new training programs. Below are examples of potential reimbursement for the costs associated with an example GME program. Table 1 provides an example of indirect medical education cost reimbursement, and Table 2 provides an example of direct medical education cost reimbursement. These examples are provided for illustration purposes only, and actual experience will vary.
Table 1 – Example Indirect Graduate Medical Education Cost Reimbursement
Table 2 – Example Direct Graduate Medical Education Cost Reimbursement
Section 131 of the Act outlines how certain hospitals with very low direct GME Per Resident Amounts (PRAs) or resident caps may have the opportunity to reset those PRAs and resident caps. The hospital should start by reviewing the guidance provided and linked here. This will allow the hospital to confirm its eligibility through careful review of the information provided by CMS – on its own. CMS has posted an extract of the Medicare cost reports from the Hospital Cost Report Information System (HCRIS) to assist hospitals in determining their eligibility. The Medicare Administrative Contractors (MACs) will not reach out to hospitals to inform them of their eligibility, nor will MACs review requests to confirm eligibility.
According to CMS, hospitals that believe they are eligible for a reset, but the HCRIS data posting shows a hospital is not eligible, have a one-time opportunity to demonstrate to the MAC that it is eligible for a reset. The hospital must electronically submit complete and unambiguous documentation, which must be received by the MAC no later than July 1, 2022. The guidance provided by CMS provides the criteria and steps that must be taken.
Hospitals that do not have a cost report posted in the HCRIS web posting, or if there is no PRA or no FTE caps reported (because the cost report has not yet been settled and/or the MAC has not yet determined the PRA or the FTE caps), must submit a request to the MAC by July 1, 2022, requesting the MAC issue a determination regarding possible reset eligibility for the PRA and/or FTE caps. Again, the request must be received by the MAC by the deadline and include complete and unambiguous documentation supporting the request.
PYA can assist organizations in determining the viability of new or expanded GME programs by facilitating strategic discussions and supporting the financial analysis related to GME programs. If you would like more information or need help with any matter involving rural health, strategy and transactions, compliance, or valuation, one of our executive contacts would be happy to assist. You may email them below, or call (800) 270-9629.
[i] https://www.regulations.gov/document/CMS-2021-0070-6388
[ii] https://mearis.cms.gov/public/resources?app=gme126
[iii] https://www.aamc.org/news-insights/press-releases/new-aamc-report-confirms-growing-physician-shortage
[iv] https://www.aamc.org/data-reports/students-residents/interactive-data/report-residents/2021/table-c6-physician-retention-state-residency-training-state
[v] https://www.aamc.org/data-reports/students-residents/interactive-data/report-residents/2021/table-c6-physician-retention-state-residency-training-state