Executive Contacts
Most inpatient hospital services for patients entitled to Medicare Part A are paid under an inpatient prospective payment system (IPPS). This payment methodology does not apply to services provided in a Critical Access Hospital (CAH), as those are paid under a cost-based methodology.
Services covered under the IPPS include:
- Room and board.
- Nursing services and other related services.
- Use of hospital facility.
- Medical social services.
- Drugs, biologicals, supplies, and equipment.
- Certain other diagnostic or therapeutic services.
- Medical or surgical services provided by certain interns or residents.
- Transportation services, including transport by ambulance.[1]
Services excluded from the IPPS are:
- Post-hospital care (payable under other prospective payment systems).
- Physician services (payable under Medicare Part B benefits).
- Direct medical education (separately reimbursed).
- Organ acquisition (separately reimbursed).
- Medicare bad debts (separately reimbursed).
Discussion
Base Rate
Standardized Amounts: The base rates used to calculate payments under the IPPS are called standardized amounts. The annual standardized amounts are intended to represent the national average cost for an average Medicare case and are based on 1981 Medicare costs, trended forward by an annual update factor. The annual update factor is often referred to as the hospital market basket and is frequently modified up or down based on various adjustments, such as changes in productivity or coding intensity (behavioral offsets).
Facility-Specific Adjustments
Differences in Area Wages: The area wage index measures the relative level of hourly wages for hospitals within each labor market compared with the national average hospital hourly wage and is used to adjust the payment rates for geographic variation in labor costs. The standardized rates are separated into labor-related and non-labor-related portions. Only the labor-related portion is adjusted by the wage index. By law, the labor-related portion of the standardized rate is set at 62% for hospitals in areas with a wage index less than 1.0. For other areas (wage index greater than 1.0), the labor portion of the wage index is adjusted annually based on the proportion of hospitals’ costs attributable to wages and wage-related costs of the prospective payment rates.
Wage Index Adjustments
Occupational Mix: The occupational mix adjustment is intended to control for the effect of hospitals’ employment choices on the wage index. These employment choices are focused on the use of registered nurses vs. other levels of nursing staff to care for patients. Unlike the wage index, which is adjusted every year, the occupational mix is reviewed and adjusted on a triennial basis. The results of that review are “carried forward” until the next review, although hospitals do have the ability to submit revised occupational mix data.
Rural Floor: Under a provision of the Balanced Budget Act of 1997, the wage index of a hospital located in an urban area of a state cannot be less than the wage index applicable to hospitals located in the rural areas of that state. Other types of wage index protection may be available to hospitals located in “frontier states” and those hospitals whose wage index is below the national median wage index.
Geographic Reclassification: Hospitals competing for labor with hospitals in a different market can request to be reclassified into the market with which they are competing. Once approved, the reclassified hospital receives the wage index of the area to which they reclassified. Reclassifications are effective for three years but may be withdrawn prior to that time frame under certain circumstances.
Inpatient Quality Reporting (IQR) and Promoting Interoperability (PI): Hospitals failing to report specific quality data receive a one-fourth reduction to the percentage increase in the market basket index, which measures the change in cost(s) from one year to the next. The update reduction is a one-year adjustment and does not affect the facility’s base rate from one year to the next.
View current IQR measures here.
The Centers for Medicare & Medicaid Services (CMS) developed the Medicare Promoting Interoperability program to encourage providers, including hospitals, to adopt, implement, upgrade, and demonstrate meaningful use of certified electronic health record (EHR) technology. Those who are not meaningful users receive a three-fourths reduction to the percentage increase in the market basket index.
The required measures under the PI program for each fiscal year are found here.
Under the Medicare IPPS, hospitals’ standardized amounts will ultimately be based on one of the following eight payment classifications:
Wage Index > 1.0 |
|||
|
1 |
2 |
3 |
4 |
|
Hospital submitted Quality Data and is a Meaningful EHR user |
Hospital submitted Quality Data and is NOT a Meaningful EHR user |
Hospital did NOT submit Quality Data and is a Meaningful EHR user |
Hospital did NOT submit Quality Data and is NOT a Meaningful EHR user |
Wage Index < 1.0 |
|||
|
5 |
6 |
7 |
8 |
|
Hospital submitted Quality Data and is a Meaningful EHR user |
Hospital submitted Quality Data and is NOT a Meaningful EHR user |
Hospital did NOT submit Quality Data and is a Meaningful EHR user |
Hospital did NOT submit Quality Data and is NOT a Meaningful EHR user |
Acute care hospitals located in Puerto Rico are paid based on different standardized amounts. There is also a separate standardized amount classification for long-term acute care hospitals.
Capital: Capital-related costs include depreciation, interest, insurance, and taxes. Hospitals are reimbursed for capital using a federal rate, which is adjusted annually. The capital rate is calculated as follows:
All hospitals subject to Medicare IPPS receive the operating and capital payments outlined previously.
Generally, the DRG operating and capital payments are considered final payments, not subject to further cost report settlement. Hospitals participating in approved graduate medical education programs, as well as those serving a disproportionate share of low-income beneficiaries, receive additional payment adjustments. These payment factors, known as the indirect medical education (IME) and disproportionate share hospital (DSH) adjustments, are intended to compensate hospitals for the incremental costs they may incur compared to non-teaching hospitals or those hospitals not serving a disproportionate share of low-income patients. These incremental costs may be attributable to extra costs associated with residents involved in patient care activity or low-income patients presenting at the hospital without adequate “pre-hospital care.”
Indirect Medical Education (IME): Teaching hospitals receive add-on payments to the operating portion of the DRG payment based on a metric known as the teaching intensity factor. The teaching intensity factor is calculated using a formula based on the number of interns and residents assigned to the IPPS portion of the facility, divided by the bed days available in the IPPS portion of the facility. Both the count of interns and residents, as well as the bed days available, are Medicare “terms of art” and defined by regulation. The actual number of residents trained may be different than those included in the calculation due to counting rules established by regulation.
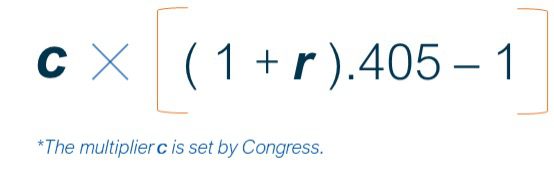
The IME adjustment factor is calculated using a hospital’s ratio of residents to beds (represented as r) and a multiplier (represented as c) in the following equation:
A teaching hospital also receives an adjustment to its federal capital rate based on the ratio of its average number of residents to average daily census. Both the operating and capital IME amounts are subject to final cost report settlement because the actual payment factors are not fully known prior to the completion of the annual Medicare cost report.
Disproportionate Share: Hospitals treating a disproportionate share of low-income patients receive additional payments intended to partially offset revenue losses from furnishing uncompensated care. The current DSH payment methodology is based, in part, on a statutory formula that varies based on the location of the hospital (urban or rural) and the percentage of uncompensated care patients, known as the DSH patient percentage.
This percentage is equal to the sum of the percentage of Medicare inpatient days attributable to patients eligible for both Medicare Part A and Supplemental Security Income (SSI) and the percentage of total inpatient days attributable to patients eligible for Medicaid but not Medicare Part A. The DSH patient percentage (DPP) is expressed as follows:
Hospitals whose DSH patient percentage exceeds 15% are eligible for a DSH payment adjustment.
Hospitals receive 25% of their total DSH payment based on this statutory formula. This amount is frequently referred to as “empirically justified DSH.” This amount is an add-on to the DRG payment, so it is case-mix adjusted.
Uncompensated Care Costs (UCC) Pool Payment: The remaining 75% is considered a UCC pool distribution and is adjusted annually to address changes in the amount of empirically justified DSH and the percentage of uninsured individuals. The UCC payment is not tied to Medicare IPPS payments. However, to qualify for the UCC payment, the hospital needs to also qualify to receive empirically justified DSH payments. The payment amount is based on each hospital’s share of the total UCC reported by IPPS facilities.
Once determined, the amount is paid to the hospitals as a flat amount per discharge, using the estimated number of Medicare discharges from prior cost report information. Each hospital’s total payment for UCC is fixed and finalized with the publication of the inpatient final rule, but the amount is subject to final cost report settlement because the actual discharges paid for a particular federal fiscal year will vary from the published estimate. This could result in amounts due to or from the hospitals.
Hospitals with at least 100 beds located in urban areas that serve low-income patients also receive a DSH adjustment to the federal capital rate. There is no separate calculation related to uncompensated care.
Patient/Case-Specific Adjustments
Medicare Severity-Adjustment Diagnosis Related Groups (MS-DRGs): Under the Medicare program, each inpatient hospital discharge is grouped into an MS-DRG, which reflects a patient’s severity of illness, complexity of service, and hospital resource consumption. The patient’s principal diagnosis and up to 24 secondary diagnoses, including any comorbidities or complications, determine the MS-DRG assignment.
There are three levels in the MS-DRG system based on comorbidities and complications—ranking highest (1) to lowest (3) as follows:
- Major Complication/Comorbidity (MCC)
- Complication/Comorbidity (CC)
- Non-Complication/Comorbidity (Non-CC)
The final MS-DRG payment is determined by the patient’s discharge diagnoses, gender, and discharge status. Each MS-DRG is assigned a weight that reflects the average cost of the services within that group compared to the average Medicare case cost. The MS-DRG weights are adjusted annually.
Transfers: Under the IPPS, MS-DRG payments are subject to reduction when the patient’s length of stay (LOS) is at least one day less than the geometric mean MS-DRG LOS, and the patient is transferred to:
- Another IPPS-covered acute care hospital.
- A post-acute care setting (not applicable to all MS-DRGs).
- A Critical Access Hospital (CAH).
For transfers, a post-acute care setting refers to:
- Long-term care hospitals.
- Rehabilitation facilities or distinct part units in an acute care hospital or CAH.
- Psychiatric facilities or distinct part units in an acute care hospital or CAH.
- Skilled nursing facilities.
- Home health, in those cases where care is related to the hospital stay and begins within three days after discharge.
- Cancer hospitals.
- Children’s hospitals.
- Hospice care.
The hospital receives twice the per-diem rate for the first day of the stay, and the per-diem rate for each additional day, up to the full MS-DRG payment. However, it should be noted that in the case of post-acute transfers, there are certain special pay MS-DRGs for which the transferring facility is paid one-half of the full MS-DRG amount plus a full per diem on the first day and one-half the per diem for each additional day, up to the full MS-DRG rate.
Outliers: In addition to the base MS-DRG payment, hospitals can receive an outlier payment for high-cost patients. While the basis of a PPS system includes an offset of losses in some cases with gains on others, offsets are not an option for extraordinarily costly cases. CMS sets the fixed-loss threshold annually so that total outlier payments for operating costs reflect approximately 5.1% of total DRG operating payments.
Hospital-specific cost-to-charge ratios are applied to a case’s covered charges to determine whether its costs (combined operating and capital-related) exceed the fixed-loss outlier threshold. The thresholds are adjusted by the area wage index and capital geographic adjustment factor before they are compared to the operating and capital costs of the case. Payments for eligible cases are then made based on a marginal cost factor, equal to 80% of the combined operating and capital costs exceeding the fixed-loss threshold (90% for burn DRGs).
New Technology Add-on Payments: Medicare makes additional payments for certain new medical services and technologies. To be considered for additional payment, the new medical service/technology, must:
- Be new.
- Be costly, such that the DRG rate otherwise applicable to discharges involving the medical service or technology is determined to be inadequate.
- Demonstrate a substantial clinical improvement over existing services or technologies.
Payments for new technologies are in addition to the DRG payment and any applicable outlier payments.
Paying for Value: Under the Affordable Care Act, CMS implemented three quality-based programs for hospitals paid under the IPPS:
- Hospital Readmission Reductions Program (HRRP)
- Hospital-Acquired Condition Reduction Program (HACRP)
- Hospital Value-Based Purchasing Program (VBP)
Under HRRP, the base payment rate is adjusted for excess readmissions. Excess readmissions are reviewed over a three-year period for:
- Acute myocardial infarction.
- Chronic obstructive pulmonary disease.
- Heart failure.
- Pneumonia.
- Coronary artery bypass graft surgery.
- Elective primary total hip or knee arthroplasty.
A readmission is an admission that occurs within 30 days of discharge from the same or another hospital paid under the IPPS. Payment reductions under the program apply to all Medicare claims, not just those related to the conditions/services noted above, and are capped at 3% of the standardized amount. The HRRP program is adjusted based on the hospital’s proportion of Medicare/Medicaid dual-eligible patients to address socioeconomic disparities across providers. The HRRP is always a negative payment adjustment.
Additional information on the HRRP can be found here.
Under the hospital-acquired condition (HAC) program, payments are reduced for those hospitals falling in the worst-performing quartile of all hospitals on measures of hospital-acquired conditions. An HAC is a condition occurring during a stay (not present on admission). Those hospitals in the worst-performing quartile receive a 1% payment reduction to the overall Medicare payment amount, not just to the standardized amount. The HAC is always a negative payment adjustment.
The HAC measures are available here.
The hospital VBP program is funded by a reduction of 2% of hospitals’ base operating MS-DRG payments (the standardized amount). This VBP “pool” is then redistributed in its entirety to all providers showing improvement toward or achievement of a measure-specific benchmark. A hospital can regain all, some, none, or more than the 2% withheld based on its quality performance. The VBP adjustment can be positive or negative.
The VBP program groups quality measures into four equally weighted domains:
- Safety
- Clinical outcomes
- Person and community engagement
- Efficiency and cost reduction
The VBP measures for the current year can be found here.
Resources
This Insight is part of our Medicare Payment Primers Series. If you would like additional information about the Inpatient Hospital Prospective Payment System or other prospective payment systems, or have questions about any matter related to reimbursement, strategy and transactions, compliance, or valuation, one of our executive contacts would be happy to assist. You may email them below, or call (800) 270-9629.
[1] Medicare Benefit Policy Manual, Pub 100-02, Chapter 1.