On November 1, 2018, the Centers for Medicare & Medicaid Services (CMS) released the 2019 Medicare Physician Fee Schedule (MPFS) Final Rule. For the first time since the Quality Payment Program (QPP, or Program) launched in 2016, changes to the Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (Advanced APMs) were incorporated into the MPFS Final Rule. Now two years in, the Program has an established foundation, and changes are generally minor enhancements, as opposed to major overhauls.
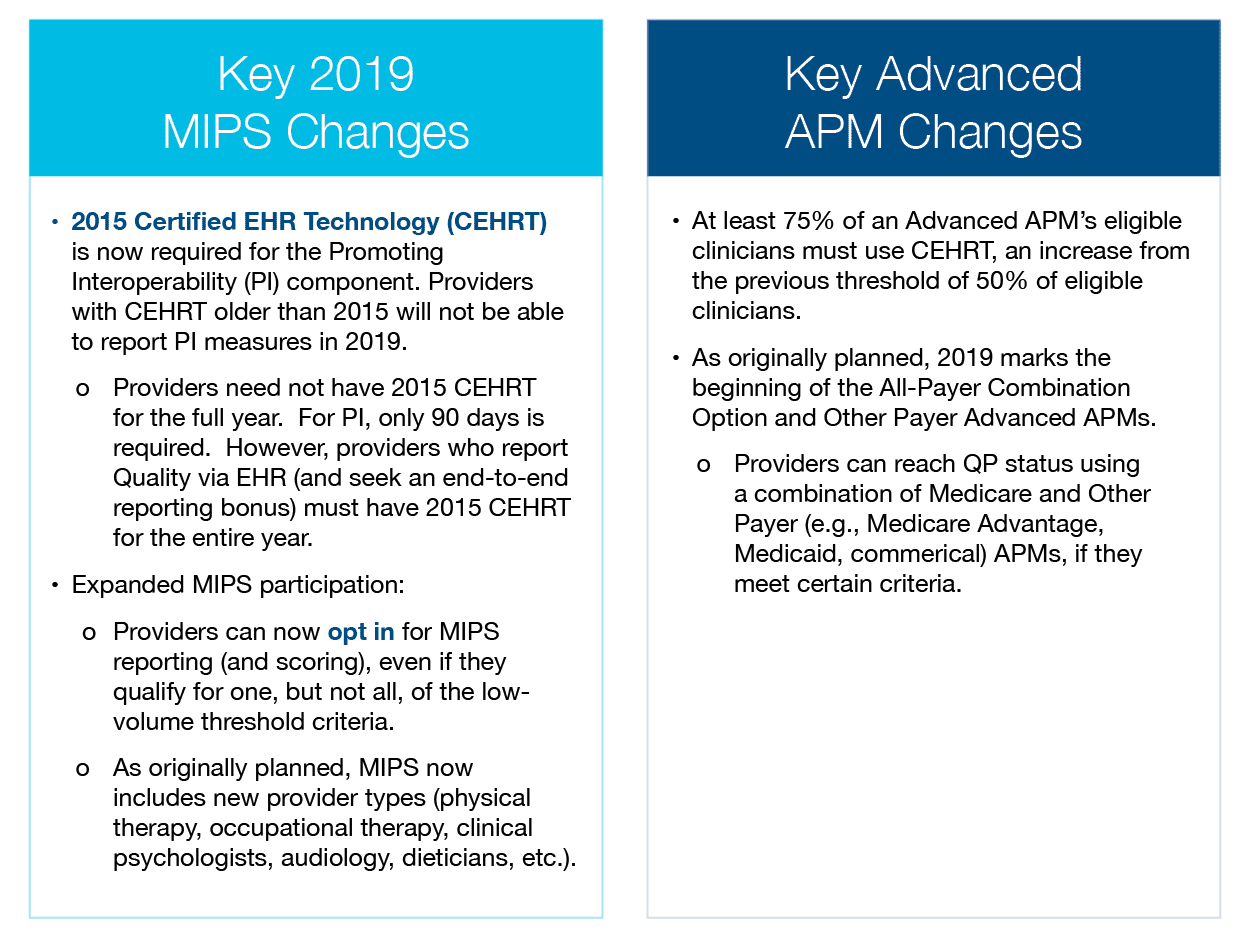
The 2019 policies, which will impact Performance Year 3, continue to steadily roll out the QPP, allowing providers time to familiarize themselves with the Program. Year 3 brings a higher MIPS point threshold, a higher percentage of fee-for-service (FFS) dollars at risk, and similar reporting requirements as the first two Program years. CMS published a comparative fact sheet with the full summary of changes. Some of the key 2019 MIPS and Advanced APM changes are outlined below:
Among other year-end priorities, providers should start thinking about their QPP strategy for 2019. PYA has outlined the following recommendations for a successful QPP Year 3 based on experience level.
Beginner Participants
These recommendations are for those with limited resources dedicated to QPP, those still unfamiliar with specific Program requirements, those who have not yet reported MIPS data and only “avoided penalties,” or those who have given no consideration to Advanced APMs.
- Recommendation 1. Familiarize yourself with ramp-up requirements in Year 3 and beyond. If your EHR is not CEHRT 2015, start working with a vendor to make this transition as soon as possible. Keep monitoring available and applicable quality reporting measures, and be prepared for the cost component to account for a larger portion of the final score.
- Recommendation 2. Create a written plan with specific category point targets (i.e., Quality, Cost, Promoting Interoperability, and Improvement Activities) to ensure all physicians and providers avoid a financial penalty. The performance threshold for 2019 is 30 total points. At minimum, make sure to report enough to meet that mark. Investigate opportunities to earn bonus points, choose measures for which you know you can succeed, and select Improvement Activities to adopt.
- Recommendation 3. Evaluate data submission methods, and choose the path that is most practice-friendly (least burdensome, not too costly, etc.). Many practices have defaulted to claims or registry reporting, which are the primary carryovers from the Physician Quality Reporting System (PQRS). These may still be the best options depending on practice size—claims reporting is only available to practices with 15 or fewer providers)— but consider alternatives, such as reporting directly through the QPP website (which is free) or via your EHR vendor.
Intermediate Participants
These recommendations are for those with some resources dedicated to QPP participation, those who have successfully reported in Year 1 or 2, those who may have earned bonus payments, or those who have given strategic thought to maximizing either their MIPS score or Advanced APM participation bonuses.
- Recommendation 1. Study 2016 and 2017 MIPS performance results and identify areas for improvement. For example, if the quality component score was low, determine why this was the case. Was it due to poor performance on the measures (low percentages) or did you select measures that had exceptionally high thresholds? Gathering this type of information will better equip you for 2019 planning.
- Recommendation 2. Set a target of 75 MIPS points to reach the “Exceptional Performance” pool in 2019. Given what we know from the 2017 QPP results, this is one of the only ways providers can see a meaningful financial reward under MIPS, with so many providers meeting the minimum requirement and avoiding penalty. There is no guarantee of earning a significant bonus even if you reach this level, but it will be beneficial for public reporting and offer the chance to earn bonus dollars.
- Recommendation 3. Closely evaluate MIPS APM or Advanced APM opportunities. If you have been successful with MIPS for a few years, it might be time to start thinking about APM opportunities, even if it is an upside-only model. With Health and Human Services Secretary Alex Azar recently commenting that mandatory bundles could return, a proactive approach toward APMs may prove to be valuable on multiple fronts.
Experienced Participants
These recommendations are for those with sufficient resources dedicated to QPP, those who have successfully reported MIPS or participated in an Advanced APM in Years 1 or 2, or those who have experience with similar value-based contracts with other payers (i.e., commercial shared savings, Medicare Advantage, Patient-Centered Medical Home, etc.).
- Recommendation 1. Search for ways to streamline and improve reporting processes (MIPS) or participation (Advanced APMs) for maximum administrative efficiency. Are you capturing and reporting the right quality measures? Have you solidified a standard process for gathering and reviewing real-time cost or claims data?
- Recommendation 2. Learn from past experiences with QPP, and proactively approach payers about additional pay-for-performance or shared savings arrangements. If you are succeeding with certain patient populations (like care management or remote monitoring), look to apply those practices to other populations too. Now more than ever, providers need to demonstrate their value to healthcare services purchasers (payers, employers, etc.). Consider sharing positive quality or cost performance measurements with patients, payers, and other providers.
- Recommendation 3. Think beyond QPP, and explore new arrangements like direct primary care. Would a provider-sponsored health plan make sense for your organization? Can you work with local community-based organizations to better meet patient needs? Search for ways to evolve and better meet the needs of your patients and community.
PYA assists organizations in understanding and complying with MIPS requirements and developing APM strategies. For more information, contact one of our PYA executives below at (800) 270-9629.
© 2018 PYA
No portion of this article may be used or duplicated by any person or entity for any purpose without the express written permission of PYA.


