Update: Since this article was first published July 20, the Centers for Medicare & Medicaid Services (CMS) distributed additional information about the option for BPCI-A participants to withdraw from the program in March 2019. We have modified the original article to reflect that new information.
On July 6, CMS made a surprise announcement regarding participation in the Bundled Payments for Care Improvement Advanced (BPCI-A) program. In addition to pushing the deadline for clinical episode selection to August 8, and for other deliverables to September 14, CMS announced that all participants will be able to retroactively withdraw Episode Initiators and/or Clinical Episodes in March 2019.
Providers agonizing over episode selections can take a deep breath. Rather than going at-risk on Day 1, BPCI-A participants will have the opportunity to review their initial performance and discontinue participation in some—or all—episodes if they don’t like what they see. If a provider elects to withdraw, it will not be financially responsible for any episode initiated since the October 1 start date.
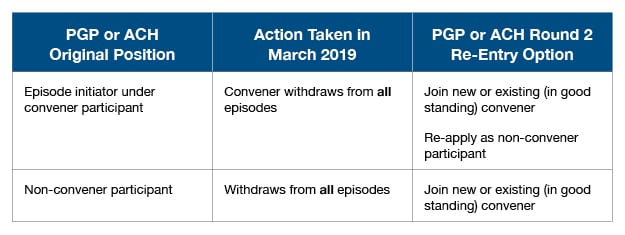
On August 1, CMS further clarified that participants who withdraw from all episodes in March 2019 are not eligible to re-apply for Round 2 of BPCI-A. Further, CMS also announced that Round 2 applications—which will take place in the spring of 2019—will be the final enrollment period for the program, covering Model Years 3-5.
What does this mean? A participant who withdraws from all episodes in March 2019 will forfeit the opportunity to be a participant in BPCI-A for the remainder of the program.
To be clear—the participant is the convener or non-convener entity that contracts directly with CMS. To re-enter the program following withdrawal in March 2019, an acute care hospital (ACH) or physician group practice (PGP) would need to do the following:
To allow applicants time to review and understand this new information, signed BPCI-A participation agreements will now be due sometime after August 8. CMS has not yet specified the exact due date. Episode selections, submitted via the participant profile, are still due on August 8.
Predicting future performance on a specific episode is challenging, especially since CMS has only provided historical claims data through March 2017. CMS’ decision to allow a six-month “test drive” will give providers more recent data on which to base their final “buy” decision. The new information about participant re-entry adds another layer of decision-making ahead of the August 8 deadline.
PYA’s BPCI-A team helps organizations with claims data analytics, episode selection, care re-design, and completion of required deliverables. For more information, contact one of our PYA executives below at (800) 270-9629.


